Important information every parent of a child with asthma needs to know
As I pass the halfway mark in my first year as a pediatric resident, I have seen many patients come through the emergency department with asthma, whether it’s for difficulty breathing or cough or chest tightness. All too often though, I find that many parents are unsure of which medicines to give when their child’s asthma is causing problems. This is usually because there are multiple inhalers at home and there can be confusion about which inhaler to give and when. With this post, we will review asthma and go over the differences between inhalers as well as when to use them.
What exactly is asthma?

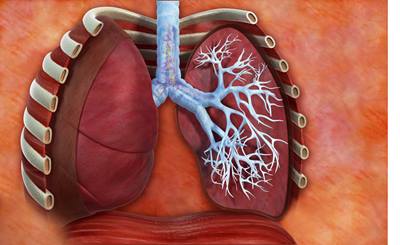
Some common words or phrases we think of when we hear the word asthma are “wheezing,” “my chest feels tight,” or “I cough a lot.” And while these are all parts of the picture that kids can have with asthma, they don’t really tell us what’s exactly going on inside their chest. . In a nutshell, asthma is a long-term, inflammatory disease that makes the airways, or the “tubes” that bring air to the lungs, smaller making it difficult to breathe.
Airways in asthma are sensitive to what we call triggers, or the spark that can cause an asthma attack. There are many triggers out there. A frequent one during the winter season is the common cold. Other common triggers are changes in the weather, cigarette smoke, exercise, hot or cold air, gastric reflux, and air pollution. Not every child’s asthma will act up to all of these triggers and some kids may only have one trigger, while others may have a combination of triggers. It’s very important to control your child’s triggers as part of preventing asthma attacks in addition to using their normal medications.
When the airways are exposed to triggers, the muscles around the airways tighten, making them smaller and making it hard to move air to the lungs. To make things worse, the area inside the airways can become swollen and plugged with mucous. The swelling and the mucous is the inflammation part of asthma. With the airways becoming smaller from both of these processes, you can see why it would be difficult to breathe when someone’s asthma acts up. Luckily, we have medicines to help with both the muscle contraction and the inflammation in asthma.
Which inhaler do I use and when?
For children with asthma, their inhalers are their best friends. Some kids only need one inhaler; others may need two. Sometimes a lot of confusion can happen when there’s more than one inhaler and this raises a lot of questions. Which one do I use every day? Which one do I give to my child when they’re sick? Why do I need two inhalers?
To keep it simple, there are two types of asthma medications that come in these inhalers. One type is called a “rescue” medication, and the other is a “controller” medication. This is often where the confusion happens. Which one do I use and when?

Albuterol to the rescue!
If you think of an asthma attack as being a fire set off by the spark of a trigger, think of the “rescue” medication as the medicine that puts out the fire. For instance, when your child is coughing a lot, or is having shortness of breath, the rescue medication “rescues” your child and tries to put out the fire. That rescue medication is albuterol. While the name of the inhaler may be ProAir, or Ventolin, or Proventil, the medication in these inhalers is still the same- it’s albuterol. Albuterol puts the fire out by reversing the muscle contraction part of asthma, making the airways bigger. When your child is having worsening symptoms of asthma, two puffs every four to six hours of albuterol can help. If your child isn’t getting better with albuterol, see your pediatrician or go to the emergency room.
Getting It Under Control
What about the controller medication? When do I use that? Some kids have asthma that is bad enough where they need two inhalers, one to put the fire out, and one to prevent the fire from happening. The controller medication is the medication that tries to prevent the fire from starting. Your pediatrician or a pulmonologist can determine if your child would benefit from a controller medication. It’s usually given to kids who are having weekly or even daily symptoms. The controller medication helps with asthma by preventing the inflammation that happens inside the airways, i.e. the swelling and the mucous. Some common controller medications that you may have heard of are Flovent, Qvar, Symbicort, and Pulmicort, to name a few. Your pediatrician can also determine which one is best for your child.
The important thing about controller medications is that they are to be taken every day. That’s right, every day, even if your child isn’t having symptoms. The best way to prevent the fire from happening is to stay ahead of it, and taking the medication every day can do just that. Typically, a child on a controller medication will take one or two puffs one to two times per day, every day. It’s important to keep in mind that while these controller medications can’t prevent all asthma attacks, they sure do help prevent a lot of them. The hope is that if the controller medication works, your child may need their rescue inhaler rarely, if at all.
Remember to be consistent
Taking the medications consistently and as directed is the key to preventing the fire that is an asthma attack. When given new inhalers, ask your pediatrician if a medication is a rescue medication or a controller, and label the inhalers as to which one is which. It also helps to take note of the color of the inhalers, as this may help in remembering if it’s a rescue or controller. Your cell phone can be helpful as well. Making a note of the color of the inhaler, the name, how and when to use it, and if it’s a rescue or a controller in your cell phone either in a note or text message can be an easy way of remembering.
Hopefully after reading this, the difference in your child’s inhalers has become clearer, and will give them a healthier and more active childhood.