Living with Gastroparesis
My name is Nancy, and today I’ll give you a glimpse into my life as I manage a chronic illness.
I’m 18 years old, and I have a disease known as Gastroparesis, which means that my digestive tract is paralyzed and unable to digest food. I have been managing this disease for about 3 years and while I do sometimes have to stay in the hospital, I have learned how to take care of many of my medical needs at home. Stay tuned throughout the day for more pictures of me as I manage my daily routine.
My day starts…
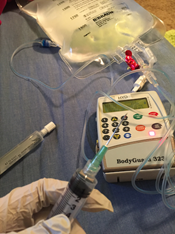
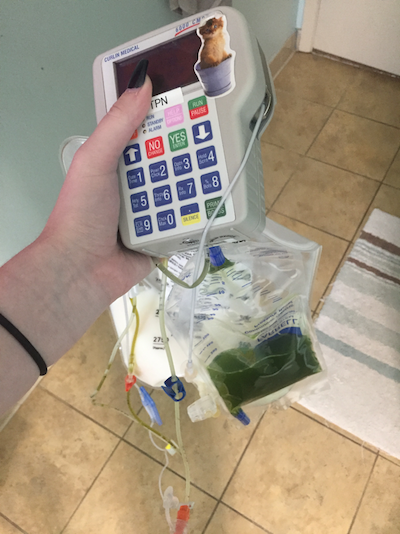
My day actually starts at night when I set up my “meal” for the following 24 hours. Between 11p.m. and midnight, I set up my Total Parental Nutrition (TPN). Because my stomach and intestines are paralyzed and can’t digest food, I am fed a special formula of chemicals that provides nutrition through my bloodstream rather than my GI tract. My doctors specially design this formula just for me to make sure my body gets exactly what I need.

Broviac Catheter
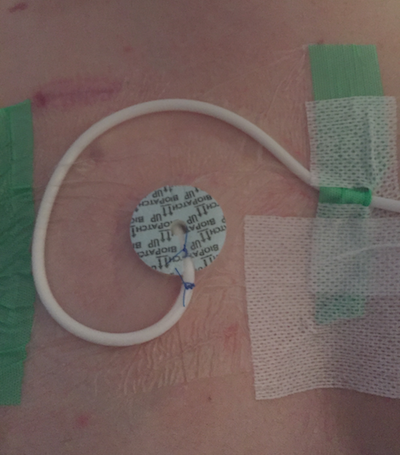 I have a Broviac catheter, which is a special tube implanted under my skin that’s like a permanent IV leading to a major blood vessel for easy access to my bloodstream. Whenever I set up an infusion or give a medication, I have to wear gloves and clean everything with alcohol to prevent infection. My TPN infusion will run overnight from an IV pole/pump by my bed.
I have a Broviac catheter, which is a special tube implanted under my skin that’s like a permanent IV leading to a major blood vessel for easy access to my bloodstream. Whenever I set up an infusion or give a medication, I have to wear gloves and clean everything with alcohol to prevent infection. My TPN infusion will run overnight from an IV pole/pump by my bed.
When I wake up…
When I wake up in the morning I have to sit up slowly, making sure my blood doesn’t pool in my feet and cause me to faint - a common symptom of my POTS (Postural Orthostatic Tachycardia Syndrome). I wake up feeling dizzy and nauseous, so it may take me some time to get out of bed.
Getting Dressed

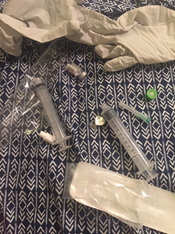
If I have somewhere to be that day, I have to get dressed. To change clothes I pause my TPN and put a sterile cap on the tubing. I also flush my line with saline so TPN doesn’t sit in it while I change clothes. This is the same thing that nurses would do in the hospital. I usually take this opportunity to give myself an IV nausea medication and flush my line again before hooking back up. It’s important for me to flush my line when it’s not running to avoid blood clots and clogs, which can be very dangerous in a central line. But I also have to make sure I don’t stay unhooked from TPN for too long, because stopping in the middle could make my blood sugar drop.
Throughout the Day…
At this point, my 12-hour TPN will stay with me in a backpack until it is finished. If I go anywhere while I am hooked up, I pack a bag with everything I’ll need to unhook in case I am out when the infusion finishes. I have to keep my backpack close to me while it’s running, which usually means putting it in the passenger seat while I drive. If my pump beeps or my infusion finishes while I’m driving, I have to pull over and address it. To unhook in public, I have to find a clean, dry surface to set out my supplies. Just like at home or in the hospital, I wear gloves, flush my line, and lock it with heparin to prevent blood clots if I will be unhooked for a long time. I also put a special green cap with an alcohol swab inside on the end of my line to keep it clean.
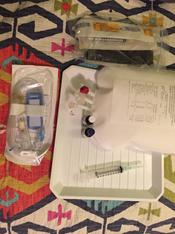
Throughout the day I also have to keep track of my vitals and g-tube output, call doctors/pharmacists/nurses regarding my TPN orders, and follow a medication schedule. These things are definitely possible to do while out, but take extra planning – especially for a person with limited energy!


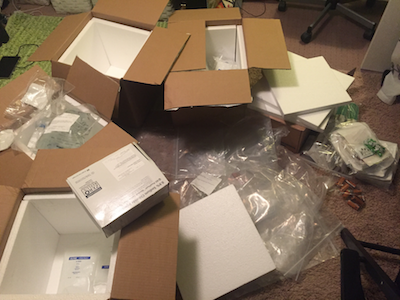
Medical Supplies
At least once a week I get a shipment of all the medical supplies I will be needing, which come in 4-5 heavy boxes. Even if I am tired, I have to unpack the boxes right away because many of my infusions and medications have to stay refrigerated. Some also need to be protected from light, or stored in other special conditions. My entire room is basically a mini pharmacy now, with all sorts of medication and supplies stored. I also have to make sure that I dispose of medical waste properly: unused meds sent to the pharmacy, needles in sharps containers, etc.

Hook up to Hydration
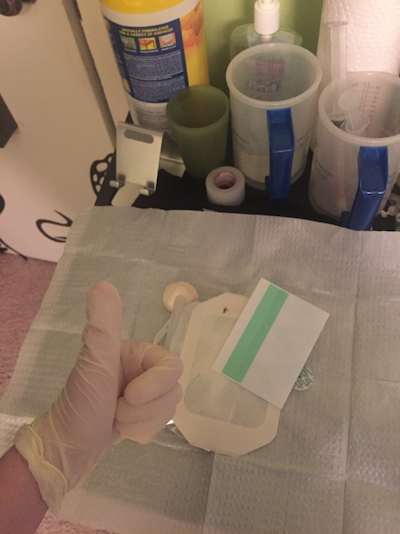 Even if I had the energy, I can’t stay out for the rest of the day after unhooking from TPN. At some point I have to go home and hook up to hydration, which runs similar to TPN on a faster pump. Whenever my IV line gets sweaty, wet, dirty, the tape is peeling off or it’s been more than a certain number of days, I have to change the dressing. Any time I do this I have to be sterile, even more so than I am while handling TPN and medications.
Even if I had the energy, I can’t stay out for the rest of the day after unhooking from TPN. At some point I have to go home and hook up to hydration, which runs similar to TPN on a faster pump. Whenever my IV line gets sweaty, wet, dirty, the tape is peeling off or it’s been more than a certain number of days, I have to change the dressing. Any time I do this I have to be sterile, even more so than I am while handling TPN and medications.
Having easy access to my bloodstream is super useful when it comes to managing my condition at home, but it also comes with huge risk. My broviac leads straight to my heart, so any kind of infection could send me into septic shock, which could be deadly.
To handle my line without dressing, I wear a mask and special gloves that have been prepared in a sterile environment, and clean with a kit that has also been sterilized. If I accidentally touch any of my supplies with a bare hand or anything that isn’t sterile, I start all over. If I want to take a shower, I have to be careful not to get my central line wet. I cover my existing dressing with gauze, tuck the line underneath, and cover that with another, waterproof dressing.
Before I go to bed, I start my day all over again.
Thank You

Thanks for allowing me to share my day with you. I hope you were able to get a small glimpse into what life is like for me with gastroparesis. I’ll leave you with this picture of me and my friend Ruby, who also has gastroparesis and manges her TPN at home.
As you can see, we’re just two teenage girls doing the best we can to do what every other teenager does- finish school, hang out with our friends, prepare for college- it’s just that we have a few extra challenges to overcome as we go.
Comprehensive Pediatric Gastroenterology and GI Surgery Services
At Orlando Health, you have an award-winning team of healthcare professionals to evaluate, identify and treat your child’s gastrointestinal (GI), liver or nutritional disorder.Learn More About Our Pediatric GI Practices
Our Pediatric GI practices have appointment times available as soon as next-day.







